Brain protein could control two major brain signatures in Alzheimer’s
Controlling or inhibiting the brain enzyme 5-lipoxygenase could be a key to controlling the two proteins — amyloid beta and tau — that are major brain pathological/lesion signatures for Alzheimer’s disease, according to researchers at Temple University.
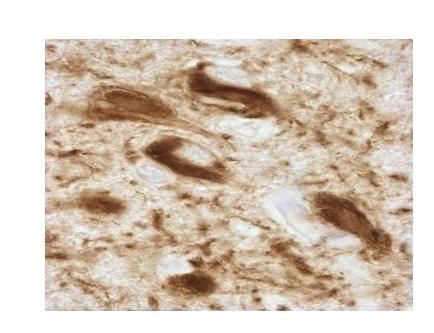
In studies led by Domenico Praticò, professor of pharmacology and microbiology and immunology in Temple’s School of Medicine, researchers found that high levels of 5-lipoxygenase in the brain corresponded with increased levels of phosphorylated tau, a protein found in the neurons of the central nervous system. Elevated levels of this type of tau protein in regions of the brain controlling memory and cognition can contribute to Alzheimer’s disease, as well as non-Alzheimer’s-related dementia called tauopathy.
Normal tau proteins act as an important component for neuronal cell health, but elevated 5-lipoxygenase levels can cause too many phosphate groups to attach to the protein, disrupting the ability of the neurons to transport a nutrient/chemical or transmit an electrical signal from one cell to another, said Praticò. This disruption can impair the brain’s ability for learning, forming new memory and other cognitive functions.
In previous studies, Praticò and his team showed that high levels of 5-lipoxygenase increase the levels of amyloid beta, which is thought to be the cause for neuronal death and forms plaques in the brain. The amount of these amyloid plaques is used as a measurement of the severity of Alzheimer's.
“Tau has been forgotten in trying to treat or control Alzheimer’s disease,” said Praticò. “So far, all of the therapies for treating Alzheimer’s have been targeting the amyloid plaques in the brain, and there have been a lot of disappointing results. A possible explanation for this is that even if you reduced the amyloid plaques, the phosphorylated tau is still there in the brain cells doing bad things.
“Now, with our latest findings, we have demonstrated for the first time that the same protein, 5-lipoxygenase, can regulate both amyloid beta and pathological tau, the two major signatures of Alzheimer’s disease in the brain,” he said.
In the earlier studies, the Temple researchers discovered that Zileuton, an inhibitor used for treating asthma, was able to block 5-lipoxygenase and reduce the amount of amyloid plaques in the brain.
Based on those results, the researchers again used Zileuton to treat mice that had increased levels of phosphorylated tau in their brains. They found that when the drug blocked or inhibited 5-lipoxygenase, the levels of this type of tau in the animal models were dramatically reduced.
Praticò said that more importantly, the reduction in phosphorylated tau through the blocking of 5-lipoxygenase coincided with an improvement in memory, learning and other cognitive functions in the mice. This could also be important in treating non-Alzheimer’s-related dementias or tauopathy.
“No one has ever shown pharmacologically that if you reduce the level of phosphorylated tau with a drug, you can reconnect those cells in the brain,” he said.
“We might now have a potential therapy that targets both amyloid Beta and phosphorylated tau in the brain,” said Praticò. “For the first time, we demonstrated that basically, with the same bullet, you can kill two birds.”
The Temple researchers published their recent studies, “The influence of 5-Lipoxygenase on Alzheimer’s disease-related tau pathology: in vivo and in vitro evidence” and “5-Lipoxygenase pharmacological blockade decreases tau phosphorylation in vivo: involvement of the cyclin-dependent kinase-5,” in the journals Biological Psychiatry and Neurobiology of Aging, respectively.
The research was funded through grants from the National Institutes of Health.