From Petri Dish to Patient
<p>In 2014, Temple researchers made a major breakthrough in the search for a cure to HIV. But their work has just begun.</p>
Photography By:
Joseph V. Labolito
Story by:
Kate O'Neill
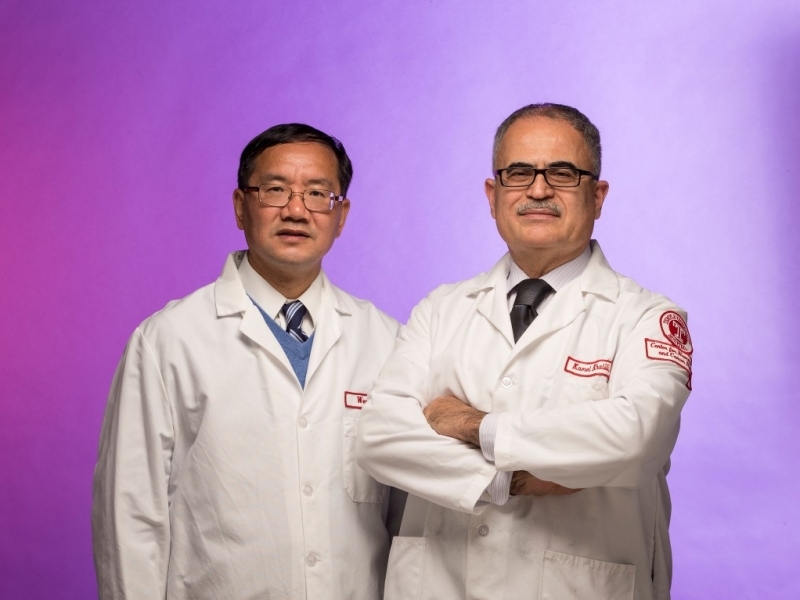
Kamel Khalili (right), founding chair of the School of Medicine’s Department of Neuroscience and director of the Comprehensive NeuroAIDS Center, and Wenhui Hu, associate professor of neuroscience, led a team of Temple researchers who eliminated HIV from human cells.
Like most Philadelphia neighborhoods, the ones in the city’s 19140 ZIP code are home to churches and schools, row houses and apartment buildings. But in many ways, 19140 is not average: It is one of the poorest ZIP codes in the city, with 43 percent of residents living at or below the poverty level. A third of adults over age 25 didn’t graduate from high school. And the area has one of Philadelphia’s highest rates of people living with HIV or AIDS.
Temple’s Medical Education and Research Building is also located in 19140, and in the 11-story building that towers over Broad Street, researchers are making headway toward solving one of the problems that affects too many of their neighbors: They are working on a cure for HIV.
Last July, those scientists published a paper describing a major step toward finding that cure—they successfully eliminated HIV from human cells. Since then, their breakthrough has been touted by media outlets worldwide and named one of the top 100 science stories of 2014 by Discover magazine.
But they were just getting started.
A TENACIOUS DISEASE
In the U.S., an HIV diagnosis is no longer a death sentence. A drug therapy called HAART (highly active antiretroviral therapy) developed in the 1990s suppresses the virus so HIV becomes a chronic condition, not an acute disease—most people treated with HAART will never develop full-blown AIDS. But there are problems with the treatment: It is expensive and often not available in developing countries. Not all patients respond to the therapy. And even for those who have access to HAART and whose virus is suppressed by it, there are terrible side effects.
“Diseases that you normally see in older individuals, such as dementia and cardiomyopathy, we see in younger HIV patients who are on stable treatment with HAART,” says Kamel Khalili, founding chair of Temple School of Medicine’s Department of Neuroscience and leader of the team of Temple researchers working to eradicate the virus.
But the main problem with HAART is that it doesn’t cure the disease. HIV remains, latent, in the patient’s cells.
“Every time you stop taking the pills, the virus becomes reactivated,” says Khalili, who is also the director of Temple’s Comprehensive NeuroAIDS Center. “The real issue is, how do we eradicate the virus completely?”
Three years ago, he posed that question to Wenhui Hu, associate professor of neuroscience. Hu wasn’t working on HIV; his research interest is the role of neurological stem cells in intellectual disability and digestive disease. But he does have expertise in genome editing, which Khalili knew would be essential to curing HIV.
Like all viruses, HIV requires a host—it can’t replicate by itself. When HIV invades a host cell, viral DNA inserts itself into the cell’s chromosomal DNA. It ultimately uses the host cell’s own mechanism to make virus particles, which leave the host cell and infect others throughout the body.
“The viral genome integrates in the host’s chromosome and stays there,” Khalili says. “The only way to cure a patient with an HIV-infected chromosome is to cleave that part of the DNA and rejoin the remaining chromosome.”
“People have said it’s impossible,” adds Hu, but he and Khalili put their heads together and began looking at a number of strategies.
In February 2013, they were focused on one genome-editing technique when Science magazine published a paper about a different technology, called CRISPR/Cas9, which scientists showed can be used to cut out the DNA of viruses and other organisms in human cells.
“Because of the expertise we have at Temple—the years and years we have been working with HIV and virology—we knew exactly what to do.”
-- Kamel Khalili, chair, Department of Neuroscience
The technique had to be modified to specifically recognize the HIV genome. CRISPR/Cas9 can act like a pair of genetic scissors, but it requires small fragments of RNA called guide RNA (gRNA) to identify exactly which part of the DNA it should snip.
“The idea was to develop a very specific guide RNA and put this gRNA along with the Cas9 into HIV-infected cells, cleave the genes, and then rejoin the DNA without any side effect on the chromosome or negative impact to the cell,” Khalili explains. The scientists also had to determine exactly which segment of the virus’ DNA to target.
“Other labs would fail or it would take them a very long time,” he says. “But because of the expertise we have at Temple—the years and years we have been working with HIV and virology—we knew exactly what to do. The only reason we’ve gotten this close is because of our knowledge and experience.”
HARNESSING EXPERTISE
When the CRISPR/Cas9 technology became available, everything was in place at Temple. “The technology and all of the individuals were here,” says Khalili. “Everything was lined up for us to do this; we just put it all together.”
Temple’s Comprehensive NeuroAIDS Center provided the infrastructure for research. Khalili, who has studied HIV for nearly 30 years, had deep knowledge of how the virus works. Hu had the expertise needed to design the guide RNA and determine the target DNA. Rafal Kaminski, a young research scientist, had experience with the cell lines they would use to test their system.
Because they didn’t know which part of HIV’s DNA would be the best target, Hu chose four different targets and designed four different gRNAs to direct the Cas9 enzyme to those targets. Kaminski then cloned the gRNAs and applied them to cells they would use for testing.
“When you start, you don’t work with the virus itself,” Khalili says, “you use cell models to test the concept. You screen clones that have been grown just for that purpose.”
Because he had been working with those cells already, Kaminski was able to easily create the hundreds of clones necessary to complete that first step. The screening showed the technique worked in simple cell lines, so the team moved on to a more complex cell culture model, which contained half of the virus. “Again, it was very easy for us to grow and manipulate these cells because we were already working with them,” Khalili says.
And again, their technique worked.
Finally, the team tested the system on cells infected with the live virus. “This was much more difficult,” Kaminski says. Among other issues, working with infected cells meant he had to be in a facility with a higher level of biosafety, “but it was also the most exciting.”
“Needless to say, none of us slept for six months,” Khalili says. “We worked on it almost 24/7 because it was so promising. And it was successful. We saw that you can convert cells infected with the virus into cells without the virus, and you can do so without disrupting other genes. The viral genome is completely gone or inactivated.”
But the technique developed by the team doesn’t just remove the virus from the cells; it protects those cells against future infection. When the researchers tried to reinfect treated cells with HIV, the Cas9 enzyme once again cleaved the virus from the DNA.
They published the results of their research in Proceedings of the National Academy of Sciences in July 2014.
“We saw what we were hoping to see and more,” says Khalili, “but we saw it in the lab in cell cultures. The next step is to take it to the clinic.”
CHARGING FORWARD
There are many obstacles between the scientists and their breakthrough technique and patients with HIV. For starters, the researchers need to develop a way to get the Cas9 and gRNA into patients’ cells. In cells in the lab, Kaminski was able to deliver the Cas9 and gRNA using methods that would either not work or would not be efficient in humans.
“Our best bet is a lentivirus vector,” says Khalili. Like HIV, lentiviruses can spread throughout the human body and infect many types of cells. Modified, safe lentiviruses that carry the gene-editing system developed by Temple researchers “will hopefully get to every place the virus is hiding,” says Khalili, where the Cas9 will snip the viral DNA.
The problem with lentiviruses is that they have a gene sequence similar to HIV, which means the scientists have to carefully design their target sequences so they don’t target their delivery system. “We don’t want to destroy the tool we will use to deliver the cure,” Kaminski says.
When they have developed the delivery method, they will test their system on cells collected from actual patients, then small animals—to make sure it is safe and efficient in an entire organism, not just cells—and finally large animals. Only then will they try it in humans.
Khalili estimates it will take three to five years to get the system from the lab to the clinic. And even then, he doesn’t know if it will work in patients. But those patients are the reason he has every intention of taking this treatment to clinical trial: More than a million people in the U.S. have HIV, and 35 million people around the world are living with the virus.
“It’s the dream of every scientist to do something that will help people, cure diseases,” says Kaminski from the team’s lab on Broad Street, which bisects the 19140 ZIP code. “That’s why we do this.”