For this emergency medicine specialist, life is all about multitasking
Maura Sammon is treating COVID-19 patients at Temple Health and managing an emergency clinic for thousands of people remotely.
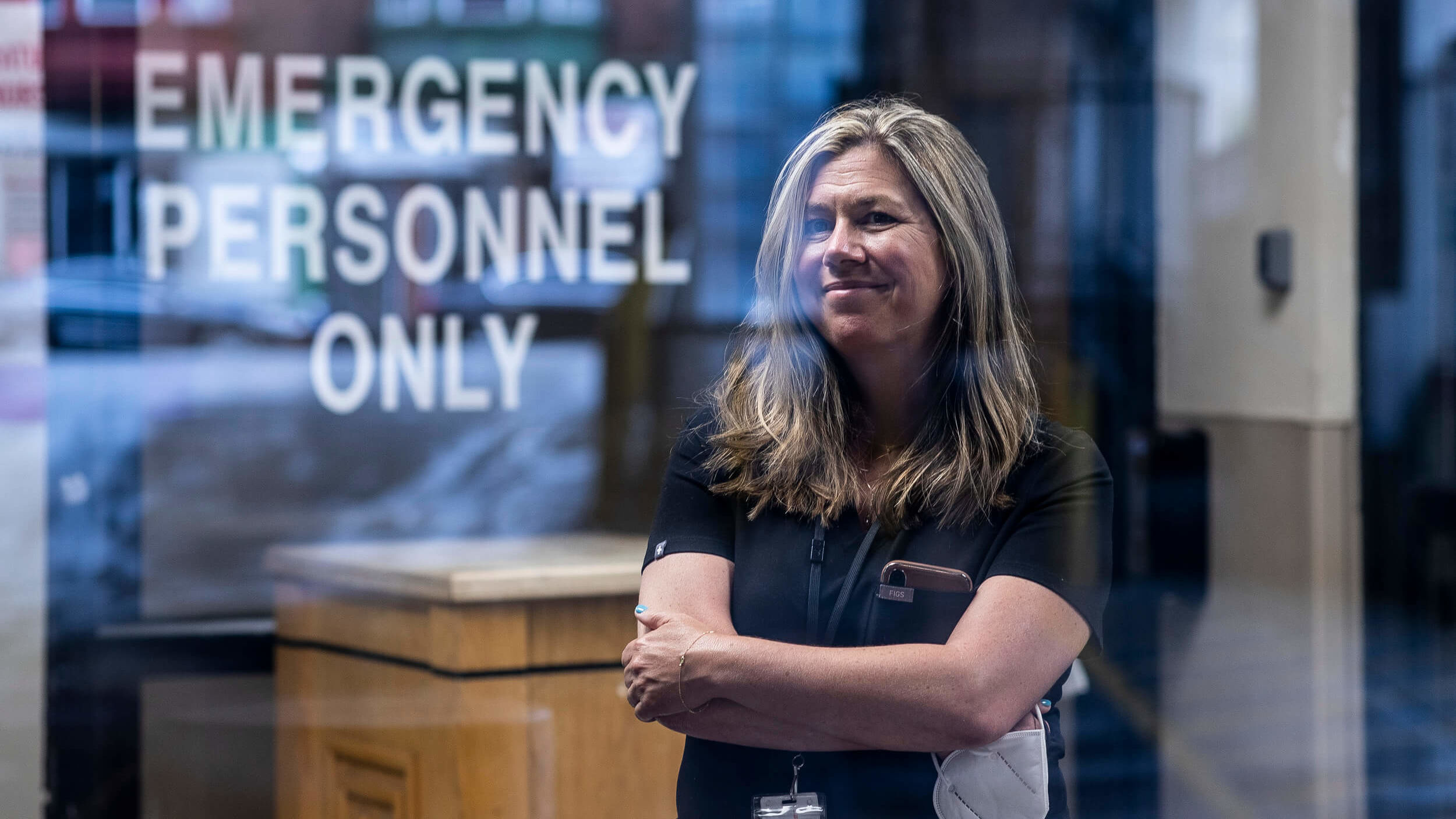
Maura Sammon, MED ’99, never stands still. An emergency medicine specialist at Temple Health, where she has been treating COVID-19 patients since the pandemic began, Sammon is an assistant professor at the Lewis Katz School of Medicine; the medical director of Global Response Management, a medical nonprofit group that functions independently of any government; and is the head of an emergency clinic on the U.S.-Mexico border, which she manages remotely. She is also a single mother.
Being an emergency room physician isn’t easy; being one during the coronavirus pandemic is even harder. “The biggest challenge is dealing with uncertainty,” Sammon said. “This pandemic is new. We are operating on limited information and we are people that are used to behaving in an evidence-based format where we can look at study x, y and z and make a scientifically well-informed decision.”
The data hospitals receive is constantly evolving, requiring staff to adapt. “One of the good things about being an ER doctor is that we’re a specialty that's a little more used to dealing with uncertainty,” Sammon said. “It's a challenge, but it's a challenge that we're able to rise to.”
It isn’t the only challenge Sammon has taken on: She also supervises an emergency medical clinic in Matamoros, Mexico, which provides care for thousands of asylum seekers and refugees. Sammon has been involved with global health projects for 15 years, working in India and Cambodia, and as an advisor to the Temple Emergency Action Corps, a student group that specializes in medical disaster relief.
She started working at the Matamoros clinic—which came into existence due to changes in U.S. immigration policy—in November 2019.
Before the pandemic, she and her colleagues were working to provide high-quality care in the most basic conditions. Now she has to do all of that remotely and “manage transmission of a highly contagious agent in an environment where people are living five to a tent.”
Sammon collaborates with a team on the ground including doctors, nurses and pharmacists— many of them refugees themselves—plus a few Global Response Management members who live at the camp full time, helping them develop safety measures to reduce the spread of COVID-19.

For Sammon and her colleagues, treating patients during the coronavirus pandemic means dealing with uncertainty. (Photo by Ryan S. Brandenberg)
Everything they do is governed by the “best better minimum” principle: “How do I use the resources that I have most effectively in order to protect the greatest number of people,” Sammon said.
Ideally, every patient who might have the coronavirus would be treated in an isolated room by people wearing personal protective equipment (PPE). But that isn’t possible. Instead, everyone wears a mask, people who share a tent are advised to sleep head to toe (to keep their faces six feet apart), and doctors are handing out shower curtains for people to use as dividers in their tents.
Sammon and her colleagues have also found innovative ways to treat non-COVID-19 patients. Recently, a child was brought in with a possible case of appendicitis. A doctor at the clinic plugged a handheld ultrasound device into his cell phone and Sammon performed a remote ultrasound, looking at the images he was getting of the patient’s appendix.
The technology “is pretty brand new and it’s really improving the quality of care we can deliver,” she said. “Many ER doctors are comfortable using ultrasound. But sometimes we have a physician there who isn’t. So I’ve trained some of the advanced practice providers we have there to do these remote ultrasounds with me.”
Sammon is constantly multitasking. While coronavirus cases are on the decline in Matamoros, they’re rising closer to home. “Numbers are going up very dramatically. We are hitting a second peak without a doubt,” she said. The best thing people can do to take the pressure off healthcare workers is to follow safety guidelines. “Just wear a mask,” she said. “The end is near. We can see the light at the end of the tunnel. This isn’t going to be forever. We can beat this.”
Sammon’s parents and sister were diagnosed with the coronavirus in June and hospitalized at Temple Health. They’ve all since recovered. She is proud of the care they received from her colleagues and from Temple as a whole.
“I am so proud to be part of this system,” she said. “I'm proud of the care that I give. I'm proud of the fact that Temple allows me to provide this care, not just locally but globally. I'm proud of the fact that we deliver this care every day without concern for who can or can't pay for it, who's insured, who's not. We have a tremendous commitment to caring for everyone.”
If there’s one thing Sammon wants people to understand about front-line medical workers, it’s their unwavering commitment. “Yes, we put ourselves at risk to care for others,” she said. “Yes, this is exhausting, both physically and emotionally. But every single person that I work with wouldn't make a different decision. We are all there because we love what we do.”
—Edirin Oputu


