Narrative medicine gives Temple’s healthcare community the opportunity to reflect
The program at the Lewis Katz School of Medicine helps doctors and medical students process their experiences and learn to be better listeners and communicators.

“I’ve always loved stories,” said Jenny Schadt, Class of 2022. “A big thing that drew me to medicine was the human aspect of it. And I think narrative medicine is a great way to tap into that.”
A student at the Lewis Katz School of Medicine, Schadt is one of the dozens of members of Temple’s healthcare community who have taken part in the university’s narrative medicine program, giving participants the space to learn to listen more carefully to the experiences of patients and then to reflect on their own experiences in healthcare—including those occurring during the COVID-19 pandemic.
Michael Vitez, the program’s director, feels medicine is intrinsically tied to storytelling: A physician’s ability to listen to a patient’s story, combined with one’s own observations and knowledge, helps doctors form a diagnosis. Narrative medicine is a natural extension of that. “It is the ability to recognize, appreciate, share and interpret stories of illness,” he said.
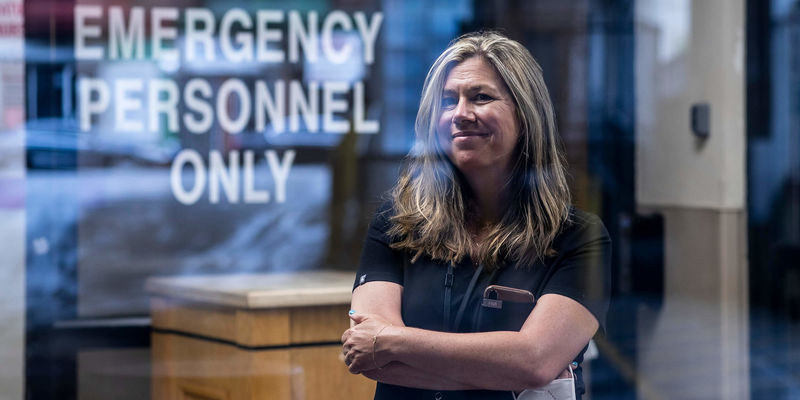
Naomi Rosenberg—associate director of the narrative medicine program and assistant professor of clinical emergency medicine—agrees. “There are things that the arts can teach us about human experience that sometimes the language of science can’t explain to us as well. For example, the opiate epidemic. We can learn the biochemical sciences of opiates and pain receptors and how the body becomes sensitized,” she said. “But that doesn’t tell us everything that we would need to know about what it feels like to live with addiction or to be the family member of someone who can’t stop using opiates.”
The idea behind the program: Studying the science of addiction might not necessarily help you understand what it’s like to struggle with the disease, but reading James Baldwin’s short story “Sonny’s Blues,” about a teacher reacting to his brother’s drug addiction, might.
The narrative medicine program—led by Vitez, Rosenberg and Douglas R. Reifler, a general internist and professor of medicine—was founded in 2016 at the Katz School of Medicine and offers elective classes for first-, second- and fourth-year medical students, as well as writing workshops for students and residents, and supports a student literary magazine, The Temple Pulse. In addition, the program runs an annual essay contest and story slam open to anyone across Temple Health, including students, faculty and staff.
In a typical student class, participants read a poem or short story and discuss it as a group. “It is so different from what they are used to,” Vitez said. “They come in off the hospital floors or out of the science library and then read a Mary Oliver poem like ‘Wild Geese.’ The first lines of it are: ‘You do not have to be good./You do not have to walk on your knees/for a hundred miles through the desert repenting./You only have to let the soft animal of your body/love what it loves.’
“I remember one intern just started crying,” Vitez said. “The rotation had been so hard, the first year as a doctor so challenging, and reading this poem was simply a release, a relief.”
Next comes a brief discussion—as doctors and medical students, not as an English class. What do they notice about the language? What lines stand out? Do they relate in any way to the poem? Then the group writes for seven minutes in response to a prompt. “My only requirement to them is that they write fearlessly and honestly. It’s extraordinary what can come out. And if they’re willing, they share. But the really important process is they just take the time to pause and reflect,” Vitez said. “People in medicine are so busy they never get seven minutes to actually stop and write and think. This is a great vehicle in terms of underscoring their own humanity, connecting with their peers and hearing one another.”
When the pandemic began, Vitez and his colleagues worked quickly to adapt and keep the program running. “It was really important to give people caring for COVID-19 patients, working on the COVID-19 floors and in the COVID-19 ICUs, an opportunity to reflect, to metabolize their experiences and process what they were going through,” he said. He chronicled the experiences of doctors and nurses and encouraged them to write and share their stories themselves.
“It was important to get those stories out there so the world could see and understand and remember what they were going through,” Vitez said. “I’m a real believer in the power of stories.”
For Schadt, writing became a way to sort through her feelings. She started writing a piece that eventually became “The Poster,” a short story about the enormous emotional toll of the pandemic, inspired by a poster someone had plastered in her neighborhood of a nurse caring for a patient, alongside the words, “If I fail, he dies.” Schadt performed it at the spring story slam last March. “Writing was one of the things that I turned to pretty early on to process [things],” she said, “[and] that story was part of the larger reflection on my time in the hospital.”
Schadt used to keep journals but she had never taken a writing class like the ones offered in the narrative medicine program until she came to Temple. “I think having those classes and experiences gave me the feeling of what it means to write just for the sake of writing. And that practice was what allowed me to return to it in the pandemic as an outlet and as a way to be more in touch with my emotions,” she said.
Narrative medicine can also help doctors become better listeners, which benefits them and their patients. “If you really listen to your patient, and hear their story, you’re much more likely to connect with and care about that patient,” Vitez said. “This will increase your own satisfaction as a physician and your patient is more likely to trust you and have a better outcome.” Listening and writing can help physicians become great communicators as well. “I tell [doctors]: improve your storytelling skills because you have such a platform and you live this incredible experience. You can influence policy, you can change minds, you can educate the public, you can do so much by telling a moving and powerful story,” he said.
And now, more than ever, it’s important to share. “We believe there’s value in learning to listen more carefully to the things patients tell us. And also in telling the stories that live inside us,” Rosenberg said. “Telling difficult stories, sharing painful moments, sharing mistakes, sharing moments of harm and joy, healing and loss, all of it is difficult to do. Externalizing some of those stories and putting them out into the world, I think, is enormously helpful for the people who do it and the people who hear it.”
Rosenberg stresses the program isn’t a substitute for counseling or other forms of intervention when needed, but she believes it does people good. So does Schadt. “A big thing that we talk about in medicine these days is resilience and burnout,” she said. “You see these really difficult things and hold them inside you. It can be tough to carry them. Narrative medicine gives people a way to not only unburden themselves but also, in hearing other people’s stories, make a connection.”
For Vitez, the program’s impact on students, faculty and staff is clear. “I believe that if you read what they write and listen to the stories they tell, you can see the value before your eyes,” he said.
—Edirin Oputu