Recreating pediatric brain on a chip could enhance the study of diseases
In collaboration with CFD Research Corp. in Huntsville, Ala., Temple engineers and neuroscientists are developing a pediatric blood-brain barrier system on a chip, which offers great potential for studying the role of the blood-brain barrier in pediatric neurological diseases and testing the blood-brain-barrier permeability of various therapeutic drugs.
The blood-brain barrier allows or prevents substances, including certain therapeutic drugs, from entering the brain. The barrier in children is more permeable than it is in adults, making it more vulnerable to neurotoxic substances that might penetrate the brain.
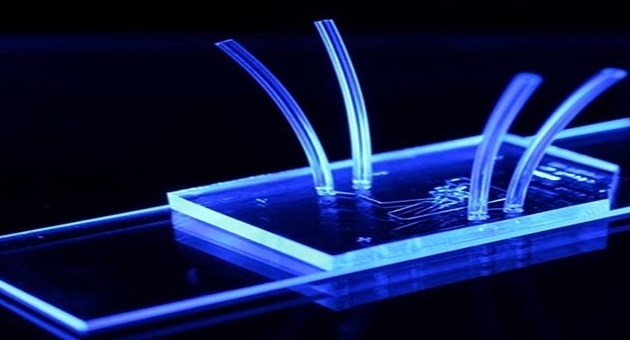
Funded by a three-year, $600,000 grant from Shriners Hospitals for Children, Temple Chair of Mechanical Engineering Mohammad Kiani—in collaboration with Barbara Krynska, assistant professor of neurology at the Shriners Hospitals Pediatric Research Center in the School of Medicine at Temple—is leading the effort, which uses neonatal rats as models for mapping brain vascular networks. Those networks are then reproduced on chips that resemble microscope slides.
Kiani’s pediatric blood-brain barrier on a chip is a dynamic system made up of a vascular compartment of pediatric endothelial cells (cells that line the interior surface of blood vessels) with fluids traveling through the vessels and a brain-tissue compartment that consists of brain cells.
Previously, Kiani had developed the technology to map the vascular networks of various animal organs. Prabhakar Pandian of CFD Research Corp., a former graduate student of Kiani’s, approached him with the idea of reproducing detailed maps on chips or slides.
“Essentially, we created a microvascular network on a chip,” said Kiani, who, with Pandian, received funding from the National Institutes of Health to develop the original chips. “But I never thought it would go beyond a one-time thing.”
Kiani then began to delve into the possible applications of reproducing vascular systems, tissues and even tumors on chips.
“Aside from all the ethical issues, doing this on chips instead of in animal models is inexpensive, reproducible and provides higher throughput,” he said. “Using these systems on chips can give you an overview of the important disease processes or permeability of therapeutics before you ever begin the more expensive animal and human studies.”
He added that researchers also might be able to use thousands of the same chips inexpensively and keep running the same experiment or varying the experiment using those chips until they figure out what is taking place.
“With these chips, we can watch everything take place in the brain vascular network in real time under a microscope,” Kiani said. “What we are seeing in them is in many ways indistinguishable from what we are seeing in vivo. If you successfully test a new therapeutic drug in this system, there is a very good chance it will also be successful in vivo.”