The Body’s Magic Bullet
A lizard can regrow its own tail after it is lost due to injury. So can a starfish with its limb and a spider with its leg. Certain types of fish can regenerate whole fins. Even a planarian, or flatworm, can grow into another worm entirely if it is cut.
Humans are capable of regeneration, too—the liver can regrow to its original size (though not its original shape) after injury or disease. And skin is regenerating itself continuously throughout our lives.
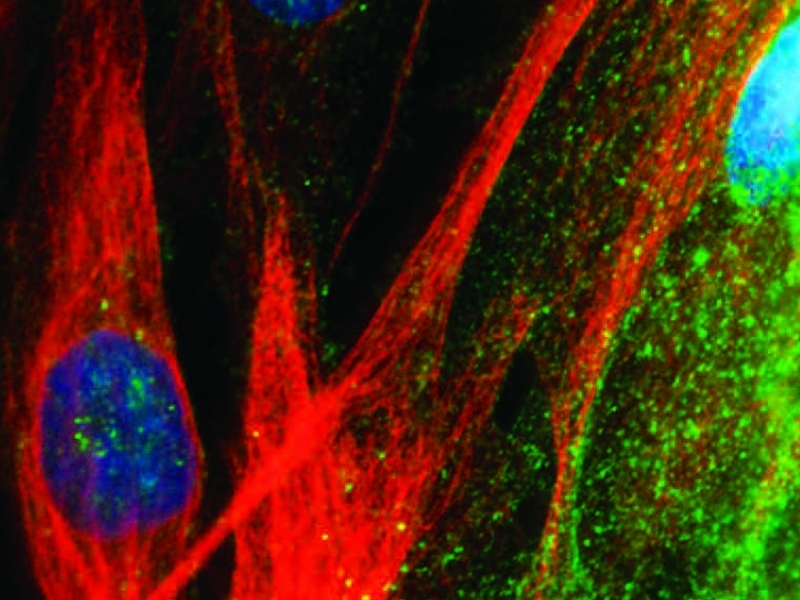
But the human body also has an often-misunderstood weapon for regeneration in the bones, blood and brain: stem cells. Those cells can divide and self‐replicate over long periods of time, and give rise to new cells in affected areas. They have long been used to combat blood cancers, such as multiple myeloma. According to the Leukemia & Lymphoma Society, more than 17,000 blood‐cancer patients had had successful stem‐cell transplants in the U.S. by 2010.
Now researchers—particularly at Temple—are investigating how to steer stem cells toward other diseases that continue to stymie the medical community.
When a heart attack, or diseases such as Parkinson's or Alzheimer's, cause cells to die off, tissue becomes incapable of repairing itself.
“Degenerative diseases are the result of cells dying in whatever tissue is being affected,” says Steven Houser, MED ’78, chair of physiology in the School of Medicine. “How do you stop the death and replace those cells? It's very hard to replace them once they die.”
Houser, who directs the Cardiovascular Research Center at Temple, likens cell death to a dead patch of grass. If it is not repopulated with new seeds, only weeds will crop up. In the body, scar tissue is the weed.
Houser and other researchers at Temple seek to capitalize on the body's ability to repair itself, to see if supplementing cells in damaged areas can help foster new cell and tissue growth.
BRAIN MATTER
Ausim Azizi, chair of neurology in the School of Medicine, has been studying cell death in the brains of Parkinson's and Alzheimer's patients for more than 20 years. Current therapies simply treat the symptoms of those diseases, but Azizi is trying to find more effective treatments and, hopefully, a cure. He believes stem cells from a patient's own bone marrow might be the key.
Though both embryonic and adult stem cells can be used for stem‐cell therapies and research, adult cells can vary in their levels of malleability. Bone‐marrow stem cells are a bit more flexible, or pluripotent—they can be manipulated to take on the characteristics of other types of cells more easily.
Azizi's research has shown that when bone‐marrow stem cells are implanted in the brain, some will adapt to the environment around them and take on the properties of neural cells. It was discovered recently that those cells release reparative and pro‐growth chemicals. “Those chemicals can make the damaged tissue grow and repair wounds a bit faster,” he explains.
Bone‐marrow cells were shown to be effective in wound care and healing more than 150 years ago, but the area was largely unexplored until the 1980s.
“People looked back and said, ‘This is a really good source of repair material,’” Azizi says. “So now, they're used largely in bone and cartilage repair—knee injuries, rotator‐cuff injuries.” He adds that chemicals from those cells also have been shown to decrease inflammation in the brain after strokes. So Azizi and his team are working with a stem‐cell therapy company and researchers at the University of Pittsburgh to see whether or not infusing those cells directly into stroke‐damaged areas of the brain will improve its function.
“They're kind of like construction workers,” Azizi says of bone‐marrow stem cells. “They're recruited from far away and come in to help out.”
HEART HEALING
Houser also studies stem cells taken from bones, to determine their effectiveness in healing cardiac tissue damaged by heart attacks. Those cells, called cortical bone‐derived stem cells (CBSCs), are even more primitive than bone‐marrow cells—meaning they might have the ability to make multiple types of cardiac tissue.
In preclinical trials, Houser and his team found some promising initial results. When the CBSCs were injected into damaged cardiac tissue, they effectively grew new blood vessels and new cardiac muscle cells, and improved the overall function of the heart.
Time is a big factor when it comes to repairing the heart after an attack. Unfortunately, extracting cells, growing them and injecting them back into a patient can take too much time, Houser says. To that end, he and his team are testing the CBSCs as allogeneic cells—meaning they can be injected from one host into another. “[The cell] will die eventually,” Houser says, “but while it's in [the body], it does good things,” such as promoting cell growth.
In another experiment in the Cardiovascular Research Center, Adjunct Assistant Professor Jon George is involved in a clinical trial examining the effectiveness of bone‐marrow cells on patients with ischemic heart disease—also known as coronary artery disease—for whom traditional therapies, such as stenting or bypass surgery, will not work.
“The idea is that those people don't have enough blood flow to the heart to allow it to work right,” Houser says of George's research. “So they would take bone marrow, isolate the cells of interest and inject them back into the heart.”
Houser operates under the theory that when cardiac cells die after a heart attack, the remaining ones must work much harder to keep the heart beating, impeding their regrowth. In order to reduce the chance of another heart attack, Houser says cell therapies can help reduce the workload.
“Data show that if you put a patient in end‐stage heart failure on a medical‐assist device so that a machine is pumping blood instead of the heart, the heart‐muscle cells get better on their own,” Houser says.
“You don't have to do anything to them. All you have to do is reduce their workload for a period of time, and they remodel themselves almost to the way they were before they had to work so hard.”
Though many stem cells can be therapeutic, some are dangerous. Learn how Temple researchers are treating some of the body's most harmful stem cells.
REGENERATE DEBATE
Though stem‐cell therapeutics show much promise for challenging and degenerative illnesses, they also are controversial. At the center of that debate are embryonic stem cells. Azizi says those are drawn from cells that have divided for eight days after eggs have been fertilized.
In 1995, the Dickey‐Wicker Amendment prohibited federal funding of research that resulted in the destruction of an embryo. And in 2001, the Bush administration placed further restrictions on that kind of research, limiting the number of embryonic stem‐cell lines that could be studied.
“It was an ideological position, stemming from the basis that life begins at conception,” says Nora Jones, CLA '01, '02, director of bioethics education at the Center for Bioethics, Urban Health and Policy in the School of Medicine. “The controversy was that it was equated to murder; you couldn't do any research that could destroy a human life.”
Additionally, according to the National Institutes of Health (NIH), some critics posit that the donation or distribution of embryonic stem cells might be conducted for profit. Despite the overturning of the Bush administration's policy in 2009, restrictions on embryonic stem‐cell lines remain. A set of research guidelines was put in place by NIH, and the ability to use embryonic stem cells varies from state to state.
Jones says that adult‐derived stem cells bypass this controversy completely. “If a cell can be taken from you and manipulated to do some sort of therapeutic intervention, then you're not destroying anything.”
Even so, Jones adds, new concerns are being raised in bioethical literature, regarding what she refers to as the “social‐justice issue.” For example, if a patient from the largely African‐American community surrounding Temple donates bone marrow—from which researchers can obtain stem cells—will that community benefit from the results of that contribution?
The newest way to harvest stem cells might put such debates to rest. Azizi highlights the importance of induced pluripotent cells. “You can take any cells that are dividing—like a piece of a skin cell—grow them in a culture dish and genetically modify them to become stem cells,” Azizi says. “During the division, those genes turn the cells into a stem cell.” But the induced cells come with a host of problems similar to other transplants, including whether or not a patient´s immune system will accept the foreign cells or kill them off.
Still, as research using stem cells continues to evolve, Jones notes that an ongoing dialogue is needed between scientists and the rest of society to address those ethical issues.
“There's a lot of research happening out there, and it's happening quickly,” she says. “As science develops, people need to have an understanding of where it's going. If we can think about what we need societally and how it can be regulated effectively some of those concerns might be alleviated.”